Tomorrow (January 6), Dr Pik To Cheung, a pediatric specialist from Hong Kong with over 30 years of experience, will be visiting International Medical Center-Beijing to offer free pediatric endocrinology consultations for children aged 6-15.
But what exactly is pediatric endocrinology? What does a consultation look like? And which child populations are susceptible to the diseases associated with the endocrine system?
We spoke with Dr Cheung to find out, and to ensure that your child gets the help they need.
Can you give us a brief explanation of pediatric endocrinology (PE)?
Endocrinology covers all the physiological systems and functions served by hormones made in various glands (gonads, pituitary gland, thyroid gland, parathyroid gland, adrenal gland, specialized islets in pancreas).
Major endocrine functions known to the general public will be sexual function (in PE, that could translate into the determination of sexual differentiation in developing fetus, precocious puberty, delayed puberty and transgender or gender dysphoria related subjects), hypothyroidism or hyperthyroidism, diabetes, hypercholesterolaemia, hypoglycaemia, menstrual dysregulation in adolescent girls, virilization in girls, gynaecomastia in boys, osteoporosis, rickets, etc.
What does an endocrinology consultation entail? What kinds of tests should a parent and their child be prepared to undergo?
Detailed clinical history relevant to the presenting symptoms (see below) will be obtained from the patient, parents and caretaker(s). Appropriate physical examination will be conducted for the list of possible endocrine disorders responsible for the presenting problem. Measurement of height, weight, blood pressure and other physical parameters will be performed. Assessing whether a child has developed pubertal features (like breast or penile enlargement, body hair and acne, pubic hair etc) is performed when appropriate.
Tests could be conducted on blood, urine or special bodily fluid/specimen for general biochemical indices, specific hormonal levels, and lipid, protein or carbohydrate metabolites depending on the likelihood of suspected clinical disease derived from the review of clinical history and physical examination findings.
As each normal endocrinological subsystem hinges on maintaining the balanced and desirable physiological functions it serves, the confirmation of an abnormal endocrinological state may entail performing special dynamic tests which usually involve repeating assessments of key indices before and after a designed test agent is administered.
In addition, imaging of body organs/structure, for example by X-ray, ultrasonography, MRI or CT scan may be warranted to confirm or rule out the aforementioned differential diagnoses.
Who should seek out an endocrinology consultation? Is this something every parent should be doing for their child, or are certain groups more at risk for endocrine complications?
Examples of problems leading to endocrine consultation include:
- short stature (long standing, recent poor height gain),
- early puberty (breast enlargement, penile growth, pubic hair),
- weight loss (especially associated with no loss of appetite)
- weight gain
- increase in urination (amount and frequency), but could be enuresis
- midline neck mass (especially with mood change, palpitation, tremor and/or weight loss)
- unusual/recurrent bone fractures
- yellowish skin lumps
Well known at-risk groups for endocrine disorders as complication are:
- Obesity
- Infant born small for gestational age (SGA)
- Those who have (and survive the harsh treatments for) childhood cancers, serious chronic inflammatory disorders requiring long term treatments
In general, it is good practice to keep a record of the developmental milestones of our children and consult the family doctor if some of these parameters are suspected to fall out of range.
Proactive discussion with doctors for possible related problems in families with strong positive history of metabolic syndrome (type 2 diabetes mellitus, hypertension, hypercholesterolaemia, obesity), dyslipidemia, endocrine related tumor, etc. is strongly encouraged in a society with advanced medical systems.
What will a parent learn from the consultation?
Parents should be able to define the scope of problems they have observed. The specific diagnosis could be clearly identified by the end of consultation, therefore the line of appropriate treatment could be outlined and a prospective plan explored and agreed upon under the guidance of the doctor. Often, the patient and parents will be given chance to get a pragmatic background understanding of such problems.
On the other hand, when the underlying cause of the defined problem is not yet firmly established, a line of workup which helps clarifying the diagnosis and relevant management plan will be suggested.
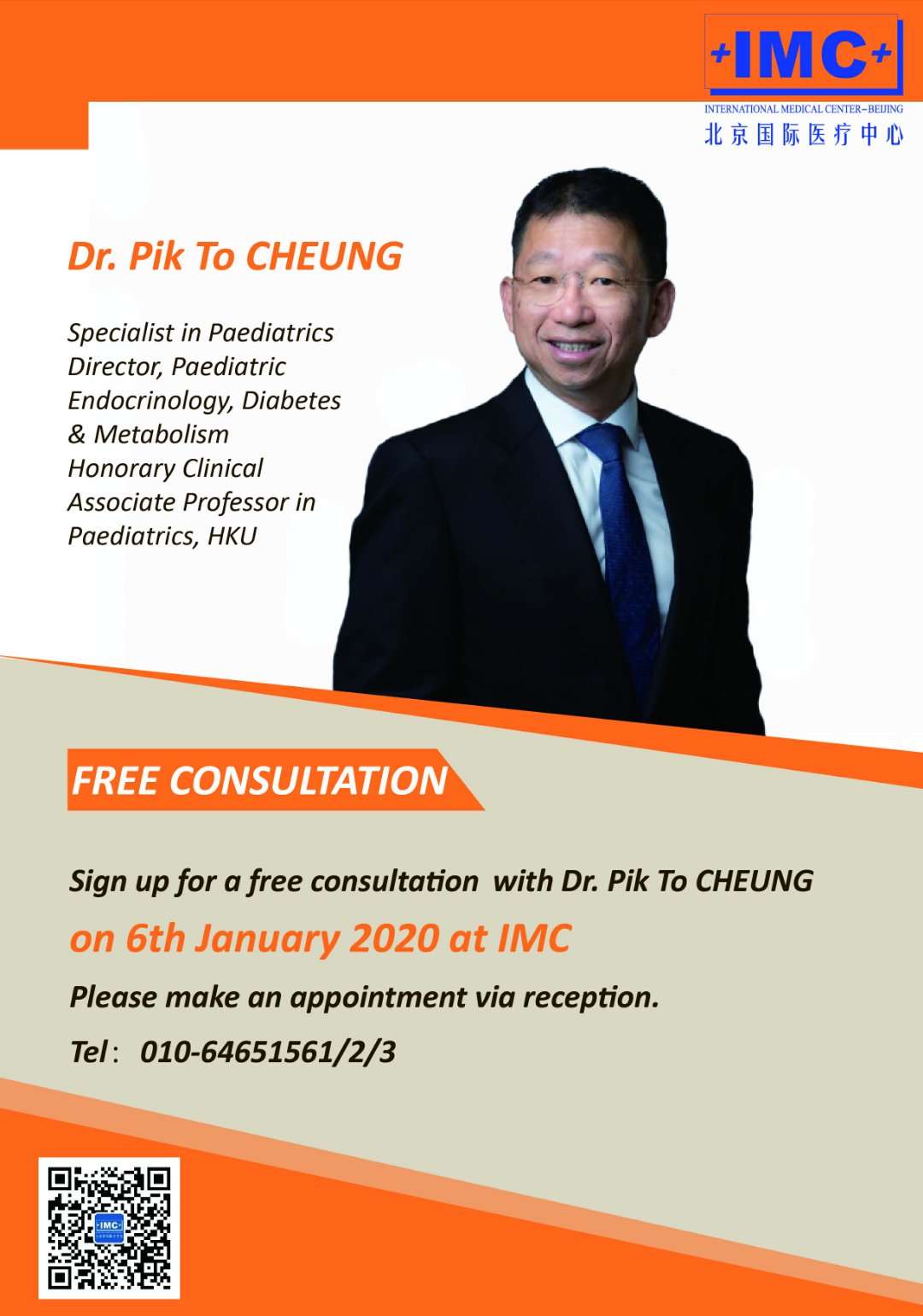
To book a consultation, scan the QR code, or call the telephone number provided
What are the risks of leaving an endocrinological disease untreated?
Certain endocrine disorders, when missed, could lead to life-threatening complications. These include type 1 diabetes mellitus, adrenal insufficiency, profound hypoglycaemia due to hyperinsulinemia, or inborn error of metabolism.
Others, if the optimal management time windows are missed, may lead to short final adult height, compromised bone health like osteoporosis with fractures, poor cardiovascular health with future heart attacks/stroke, and increased morbidity related to the primary endocrine problem.
What are the root causes of endocrinological diseases? What preventative measures can be taken to mitigate the onset of these diseases?
For a whole range of specific PE disorders, the root cause could be mutation of one single gene.
Examples could be genes involved in regulating the development of sex glands (gonads), thyroid or parathyroid gland, pituitary gland, endocrine pancreatic functions or bone metabolism.
In a subgroup of other PE disorders, it could be autoimmune in nature (for example, type 1 diabetes mellitus, Grave disease, Addison’s disease etc)
Yet some others could be nutritional, tumor, trauma, infection or inflammatory in origin.
Not many endocrine disorders are preventable. Notable examples will be obesity related complications like type 2 diabetes mellitus.
Are you seeing a rise in pediatric endocrine complications? If so, why?
There is a worldwide trend in rising incidence of type 1 diabetes mellitus. It must be related to environmental factors yet to be clearly identified.
Rising incidence of type 2 DM witnessed by us in Hong Kong and mainland China corresponds to increasing rates of childhood and adolescent obesity.
We have to take care of more endocrine complications in kids who have survived their cancer and serious haematological or chronic inflammatory diseases (mainly because of the successful treatment for their primary medical problems)
You’re based in Hong Kong, why is it important to bring these services to Mainland China?
I have witnessed strong, steady development in paediatric endocrinology all over mainland China in these past two decades. Despite that, I realize there continues to be significant demand from families coming over to Hong Kong for such service. This is not convenient for most families because of significant travel involved. I aim at providing an alternative option of bringing quality evidence-based practice closer to families who treasure our premier personal care in this field by establishing a workable system at BJIMC. Once this runs smooth, additional paediatric sub-specialties with similar conviction will be made available through BJIMC.
IMC is located at S-106/S-110 Beijing Lufthsansa Center, No.50 Liangmaqiao Rd, Chaoyang District.
Photos: Clinicaladvisor.com, IMC




