The sheer joy of finding out you are pregnant. The utter delight when you are able to scream it to the world, usually after your 12-week ultrasound. Everything is going swimmingly. 16, 17, 20: each week is proudly ticked off while the bump (and butt and boobs, but who cares right?) gets rounder and bigger.
But then, for a million and one different reasons – and sometimes without warning – this baby is coming out… way before the 40-week gestational period.
This nightmare scenario happened to one of my best friends living in the Netherlands over four weeks ago. She was pregnant and ecstatic. Everything was going so well for her and the baby. Then suddenly, whoosh, her water broke at 25 weeks gestation, with absolutely no warning. In total panic, she was first rushed to a local hospital and thereafter transferred to a bigger one in Rotterdam. After four days in the hospital, she went into labor and gave birth to a perfectly formed but oh-so-tiny baby boy.

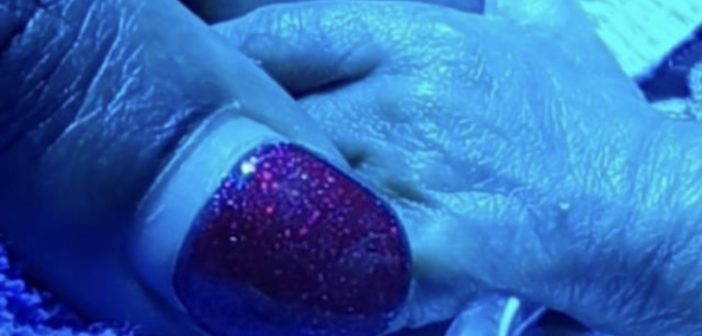
There are few things worse than your child being unwell or unhealthy. For a new mum, holding your baby for the first time is a moment dreams are made of. Doing this while the baby is attached to all manner of machines, tubes with monitors, and beepers going off every single minute can be a nightmare, to say the least.
Who is a premature baby?
A baby is considered premature or pre-term when born alive before 37 weeks of pregnancy. There are stages of prematurity in births: Late preterm is when your baby is born between weeks 34 and 36 of pregnancy. Moderately preterm is when the baby is born between 32 and 34 weeks of pregnancy. Very preterm babies are born at less than 32 weeks of pregnancy, and Extremely preterm babies are born at or before 25 weeks of pregnancy.
In most countries, babies born at less than 19 weeks are considered unviable, unlikely to survive, and doctors will generally discourage any form of resuscitation.
An estimated 15 million babies are born too early every year, according to The World Health Organization. That is more than one in every ten babies. Thanks to advances in medical care though, babies born very prematurely are now more likely to survive than ever before. Of the estimated 15 million, approximately 1 million die due to complications of pre-term births but, even if this is still a dire number, it is a testament of hope for parents going through NICU with their little bundles.
NICU in China
We asked Dr. Wennie Balawis, MD, a pediatrician from Oasis Hospital to tell us more about NICU procedures and guidelines in China.
- “When it comes to newborn resuscitation, China follows the standard international guidelines; the same as those from the American Heart Association (AHA) Neonatal Resuscitation. The two vital characteristics that determine the need for initial steps of resuscitation among newborns (both preterm and term babies) are: Breathing Problems and Heart Rate < 100 beats per minute.
- It is important to note that in local hospitals in China, parents are normally not allowed inside the NICU due to a different physical setup of the care units.
- In private hospitals like Oasis, parents are allowed to visit their babies in NICU 24/7. Visitation is only withheld for a certain period if there is a special procedure that has to be done in the NICU. There are also full parental support services like lactation nurses, on hand 24/7. Parents are also part of the medical team and are kept abreast of their child’s treatments and development through progress reports done at least twice a day (morning and evening). The treatment process and treatment options are also discussed with the parents and they participate in the decision making.
- Just like in most hospitals in Europe and America, bonding techniques like kangaroo care are allowed in private settings like Oasis Hospital’s NICU. Kangaroo care helps in establishing bonding to the parents, contributes to the success of breastfeeding, helps in thermoregulation, and helps the parents gain more confidence in caring for their baby, among other benefits. In certain circumstances when the baby’s condition is very unstable and kangaroo care is not possible, parents are still encouraged to visit the baby, touch, talk, or sing to them.
The NICU lingo
On most days, doctors and nurses speak a language that you and I won’t really grasp (a bit like Chinese – unless you are Chinese or a doctor, of course).
One of the most overwhelming things my friend has had to contend with while her baby is in NICU has been the sheer amount of information and the medical lingo she and her partner hear every single day, especially during their first week in the hospital. While it is of course important to keep parents abreast of every single development, it can be quite staggering for any new parent with a baby in potential danger.
She had to quickly learn what “bradycardia” (slower than normal heart rate), “intubation” (inserting a tube in the throat to aid breathing) and “Apnea” (temporary suspension of breathing) mean, among other medical terms. Currently, she knows what each machine is doing and what the colors, codes, and beeps mean.

Decisions in NICU
In Africa where I am from – and probably many other cultures – death is not something we talk about too openly. If someone has a terminal illness or is really sick, there will be no “straightforward” discussions about how many months or days one has left and what decisions have to be made. In Europe and other Western cultures, they will tell you straight up about all the possible outcomes and scenarios of an illness or a medical situation – the good, the bad, and the ugly. With my friend, all the best and worst-case scenarios were laid out, right up to the, “In case the baby doesn’t make it, do you still want to hold him or not?” There were also decisions over which medication they could consent to, medical trials they could participate in, and so forth. Most of the medical decisions are of course handled by capable medical professionals.
Finally Going Home

Premature babies are generally expected to stay in the NICU until their organs develop enough to stay alive without medical support, weigh at least 1,800 grams, can breathe on their own, breastfeed or bottle-feed by mouth, and maintain their body temperature and body weight, usually all in tandem. If, for example, a baby’s weight criteria is met but still require oxygen, discharge planning will change. Readiness and ability of the caregivers to take care of the baby after NICU discharge is also considered before discharge.
As expected, the first weeks were overwhelming for my friend, what with Covid-19 restrictions and the fear of infections in the hospital. Although still in NICU, the baby is with one of the best medical teams in the Netherlands and has made incredible steps in his growth and development, and we are all very hopeful he will be home in no time.
And hopefully, many in the same situation will continue to make progress.
KEEP READING: Pregnancy Diary: Unpacking Your Beijing Hospital Go Bag
Images: Unsplash, Rebecca Nassali, Pexels